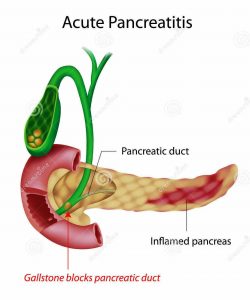
Acute Pancreatitis Causes
Gallstones and Alcohol are two major risk factors for acute pancreatitis. In few cases no cause is identified that is called as idiopathic pancreatitis. Rare causes are toxins, drugs, raised serum calcium level, hypertriglyceridemia., annular pancreas, choledochal cyst
 Acute Pancreatitis Symptoms
Acute Pancreatitis Symptoms
Stomach pain localized to upper abdomen radiating to back is the most common symptom. Nausea and vomiting are common. Patient may develop respiratory distress and decreased urine output
Acute Pancreatitis Diagnosis
Raised serum amylase and lipase level with typical pain abdomen is sufficient for diagnosis. CECT abdomen is done when there is doubt of diagnosis. If there is no doubt about diagnosis then CECT abdomen is done after 72 hrs of abdomen pain. Pancreatic necrosis if there develop till 72 hrs. CECT also show other peri-pancreatic complications
Pancreatitis Treatment
The main stay of treatment is symptomatic and supportive. I.V fluids and Oxygen therapy is given. Patient is encouraged for oral intake if there is no vomiting. TPN should be started if persistent vomiting. Nasojejunal feed can be started. There is no role for prophylactic antibiotic
Pancreatitis treatment at home
Mild pancreatitis can be treated at home. Patient oral intake should be good. Patient require good analgesia. If patient cannot be managed at home due to excess vomitting and pain then patient should be shifted to hospital where iv fluid supplement can be given
Can Pancreatitis be Cured
Acute pancreatitis is a self resolving disease which need supportive care. Recurrent episode of pancreatitis can be prevented by treating the cause of pancreatitis. In case of biliary pancreatitis, cholecystectomy will prevent recurrent attack of pancreatitis. In alcohol induced acute pancreatitis, stopping alcohol intake will prevent further episodes
Indications of Surgery in Acute Pancreatitis
Pancreatitis is a medical problem and mostly treated conservatively. In the initial phase the indication of surgery are bowel perforation & bleeding which are rare complications
In the late phase pt may require necrosectomy for infected pancreatic necrosis. It should be done after 4 week of onset of pain abdomen when the pancreatic necrosis is well demarcated and chances of complications are rare
Pseudocyst Pancreas
Pseudocyst Pancreas occur most commonly following acute pancreatitis. It occurs in chronic pancreatitis also. It is fluid collection around peri-pancreatic tissue. Following acute pancreatitis there is disruption in pancreatic duct which causes pancreatic juice to accumulate around pancreas and pseudocyst is formed. It is called as pseudocyst as there is no definitive lining of the cyst. Most of the pancreatic pseudocyts resolve following acute pancreatitis. A very few cysts persists and increase in size and causes various symptoms depending on the locations.
Diagnosis of Pseudocyst Pancreas
Ultrasound is the fist investigation as it is non-invasive and readily available. Ultrasound will detect pseudocyst, its size and relation to surrounding structures. MRI is the investigation of choice to choose the management part. If MRI show that cyst contents are predominantly liquid that endoscopic drainage is done. If there is solid component in the cyst on MRI, then surgical drainage is best
Symptoms
When the pseudocyst compress over the surrounding structures it causes symptoms. Symptoms include pain when pseudocyst increases in size. It causes vomitting when it compress over the stomach and duodenum
Surgical Management of Pseudocyst Pancreas
When the contents of the cyst are solid, Surgical management is the treatment of choice. Depending on the location of cyst either cysto-gastrostomy or cysto-jejunostomy is done. Cysto-duodenostomy is rarely done. These surgical procedures are now most commonly done by means of laparoscopy. Advantage of laparoscopy being minimal incision, less pain in the post-operative period and early recovery
Endoscopic Management of Pseudocyst Pancreas
When the cyst content is mainly in liquid form, Endoscopic management is treatment of choice. The most commonly endoscopic procedure performed is endoscopic cysto-gastrostomy
Role of Cholecystectomy in Idiopathic Pancreatitis
The occurence of two or more episodes of acute pancreatitis is recurrent acute pancreatitis. It is classified as idiopathic RAP when we cannot found any cause after a bundle of investigations. The incidence is 10-30%
The initial evaluation includes drugs history & family history of pancreatitis, Lab tests (Serum calcium,LFT & triglyceride level), USG abdomen, CECT Abdomen and MRCP
The relapse rate after first episodes varies from 14% to 24% in different studies. The rare causes include sphincter of Oddi dysfunction (SOD), pancreas divisum (PD), annular pancreas,a choledochocele, hereditary pancraetitis, Biliary sludge
Various tests have been described in literature to investigate further which include microscopic bile examination (MBE), genetic testing, ERCP with sphincter of oddi manometery, MRCP-S ( Secretin enhanced MRCP), EUS. Among all these tests EUS has emerged as diagnostic tool of choice for these patients
Various studies says EUS identified additional diagnostic information in most of these patients . The most common etiology found is microlithiasis missed on Ultrasound & MRI.It should be done after a single episode of pancreatitis after 4 weeks when the inflammation has settled down and chances of false positive diagnosis of biliary pancreatitis is also reduced as during initial phase of pancreatitis patient is in fasting stage which can also induce GB sludge
Role of prophylactic cholecystectomy is controversial, Yes if EUS after one month shows biliary sludge or microlithiasis. As the incidence of biliary sludge is more than 60% and EUS is not readily available and cholecystectomy is safe procedure, Patient can be counselled and may be advised cholecystectomy to prevent further epiosdes of pancreatitis which sometimes may be life-threatening

